Should You Be Heat Training Year-Round?
“Coz you know and i know
It's gonna be a hot summer
And you know what
It's gonna be an even hotter winter
And I ain't even talking about the weather”
Heat training is cool. It has been described as the ‘poor person’s altitude training’ and there are more Youtube videos than I can count with someone wearing one too many layers and leaving the fan off for their indoor training session. It is no secret that being adapted to the heat allows for better performance in hot environments. The evidence on that is unequivocal. This article is therefore not here to argue that point, nor is it intended to advise on heat training protocols themselves.
What this article will address however is the question as to whether the beneficial adaptations elicited through heat training justify employing this strategy year-round. Potential short cuts to big gains, or novel methods to unlock those few extra percentages get a lot of attention, but the true story isn’t always so straightforward.
I start with describing the adaptations gained from heat training, followed by the potential benefits these can imply for an athlete, particularly one practicing ultra-distances. Then, some important practical considerations are addressed before I give my hot take to conclude.
Dizzee may not have been talking about the weather, but is he referring to his training strategy for top physical performance? Well, fix up, look sharp as we are going to find out whether it should be a hot winter for us all, or whether he is jus’ a rascal and a bit, erm, bonkers.
Adaptations from Heat Training
Effectively executed heat adaptation protocols can greatly improve athletic performance in hot conditions. For just one example, Karlsen et al. (2015) found that with two weeks of heat acclimatisation, a group of nine trained cyclists were able to complete a 43km time trial in 36°C conditions with only a 2% drop in power compared cool conditions, whilst acute exposure provoked a 16% drop in power output.
The adaptations that occur through acute exposure to heat stress via this acclimatisation process include a number of physiological responses, which can be split into two categories, as described by Nybo et al. (2022). The first are non-hematological, which primarily involve the increased thermoregulatory capacity associated with improved sweat gland function. The second adaptations are hematological, mainly focused on changes in hemoglobin mass (Hb-mass), total blood volume and blood plasma volume. Enhancing Hb-mass is crucial for aerobic exercise performance as it can elevate the blood’s oxygen carrying capacity and increase the heart’s pumping capacity.
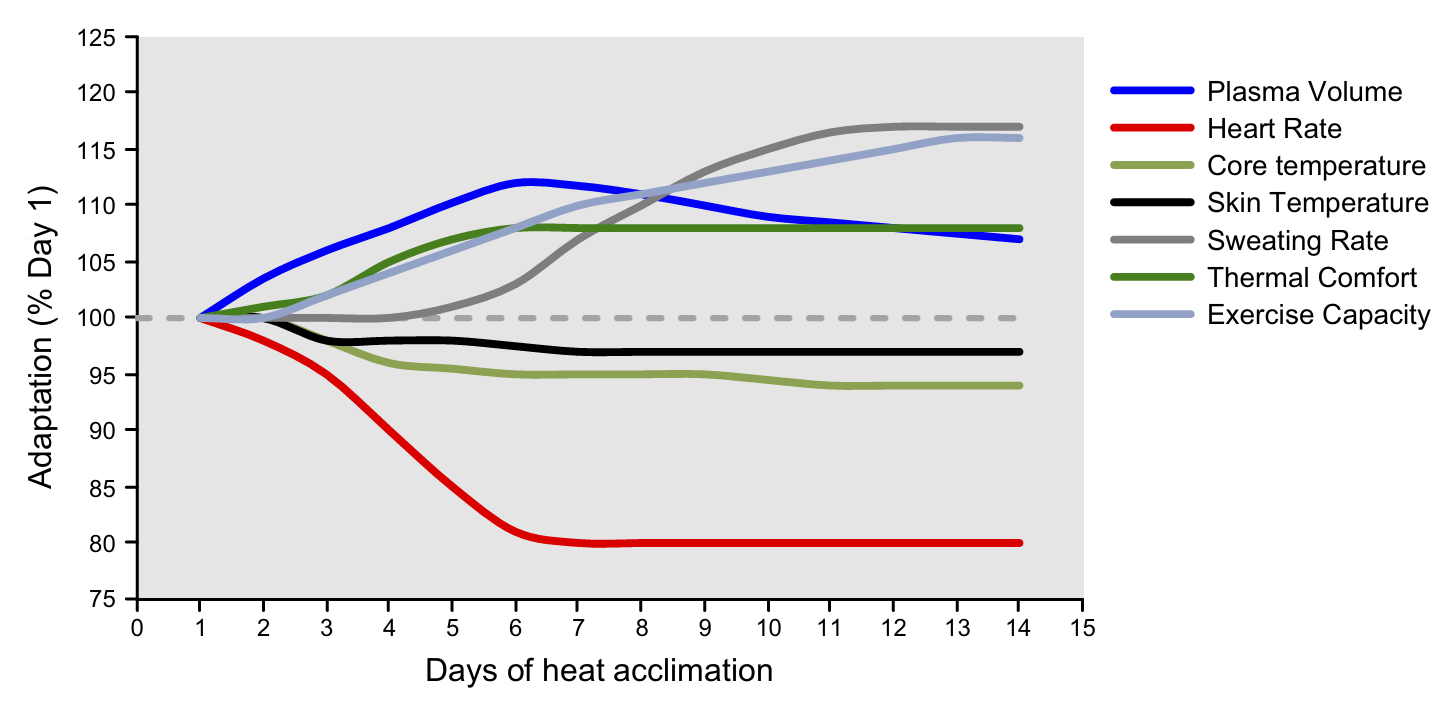
Non-hematological adaptations are generally experienced within short periods of heat stress exposure, especially within endurance trained athletes. Just 1 to 2 weeks is sufficient to see increases in maximal sweat rate, which subsequently lowers the resting core temperature and reduces the threshold for the onset of sweating. These thermoregulatory enhancements therefore allow for greater exercise capacity in environments where heat stress is the limiting factor, over and above an athlete’s aerobic capacity. The timescales associated with these adaptations are illustrated in the below diagram by Périard et al. (2015). They suggest that heat adaptation begins on the first day of exposure and that 75–80% of the adaptations occur in the first 4–7 days. The magnitude of these adaptations will be dependent on the initial level of acclimatisation, the environmental conditions, exercise intensity, and the acclimatisation regimen utilised.
Time course of adaptations to heat stress (Périard et al., 2015).
As for hematological adaptations, the evidence points to a requirement for longer term heat acclimatisation. Somewhat akin to altitude exposure, where red blood cell formation requires weeks of time to develop.
Potential Benefits of Heat Acclimatisation
Non-hematological adaptations to heat acclimatisation are those most relevant if one is to exercise in hot environments. What we are more interested in though is why it could be beneficial to be heat adapted for exercise in cool conditions year round.
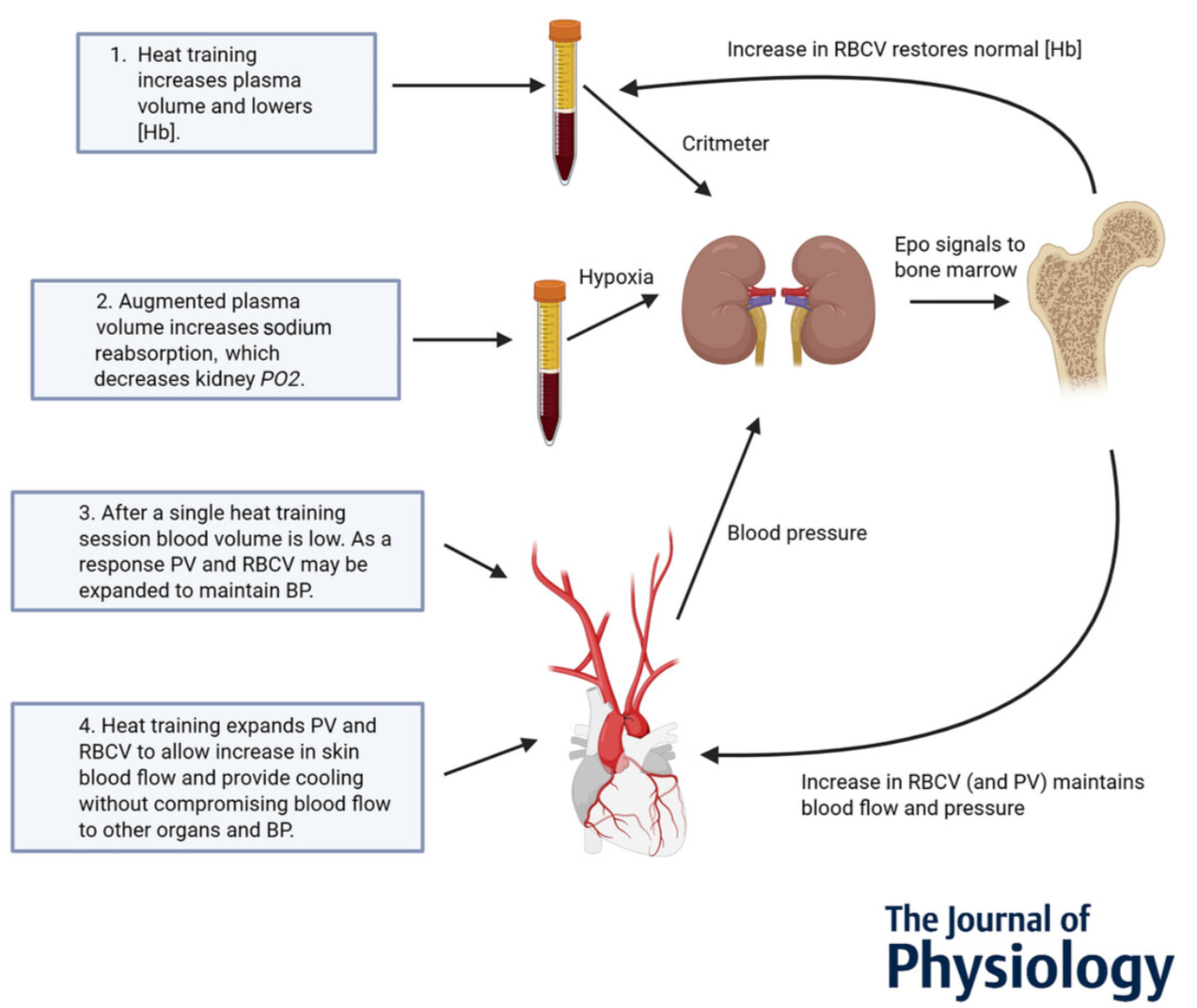
Ronnestad et al. (2022) highlight that aerobic exercise performance relies partly on a high maximal oxygen uptake (VO2 max), which in turn is associated with a high Hb-mass. Enhancing Hb-mass through heat training could therefore be beneficial to performance. The pathway to increase red blood cell volume with heat training has yet to be verified (Lundby & Robach, 2025), although several hypotheses have been proposed (see below diagram). One of these is that augmented blood plasma volume is registered by the kidney, which then increases natural EPO production and thereby red blood cell volume might be increased in an attempt to maintain hemoglobin within a normal range. This increases total hemoglobin mass and even after plasma volume reduces, the body will be left with elevated levels.
Proposed mechanisms for red blood cell volume/total haemoglobin mass to become augmented with heat training (Lundby & Robach, 2025).
“Heat acclimation improves exercise performance” is the title of a study by Lorenz et al. (2010) which appears to have really ignited interest in using heat adaptation as a means to enhance performance in all conditions. They subjected 12 trained cyclists to tests of V̇O2 max, 60 minute time-trial performance and lactate threshold, in both cool (13°C) and hot (38°C) environments before and after a 10 day heat adaptation program (50% VO2 max at 40°C). An 8 person control group also completed the exercise protocol, but at cool conditions. They found that heat acclimatisation increased all performance markers by 5-8% in hot conditions, but also by a significant 5-6% in cool conditions. The control group had no changes in performance parameters.
Cardiorespiratory and performance changes as a percent change from the preacclimation trials in both environmental conditions (Lorenz et al., 2010).
The factors they propose to account for these improvements in aerobic exercise performance in cool conditions include, amongst others, reduced oxygen uptake at a given power output, muscle glycogen sparing, reduced blood lactate at a given power output and blood plasma volume expansion.
Other studies, including those by Ronnestad et al. (2022) and Lundby et al. (2023) have also drawn this link between heat adaptation and performance in cool conditions in trained individuals. In the Lundby et al. (2022) review, they note that across all of the 5 week heat training interventions their group has completed, they have observed a ~3% increase in total Hb-mass and increased average power output during 15-30 minute time trials. However, and importantly, the control group in these experiments also improves their time trial power output, so there was no significant difference. An important distinction that we will come back to later.
The picture isn’t that straightforward though. There are equally numerous studies finding no connection between heat adaptation and performance. For instance, Mikkelson et al. (2019) subjected 12 cyclists to a prolonged heat adaptation protocol of 5.5 weeks, alongside a control group of 9 cyclists who followed the same protocol in cool conditions. VO2 max, blood volume and 15 km time trial performance were assessed in cool conditions (14°C) during a 2 week lead-in period, as well as immediately pre and post the intervention. Acclimatisation of the heat-subjected group was demonstrated through lower sweat sodium, reduced steady-state heart rate and improved submaximal exercise endurance in the heat. However, when tested in cool conditions, both peak power output and VO2 max remained unchanged for the heat group and, although time trial performance improved, a similar outcome was observed in the control group.
Mean power output in watts and 15km time trial performance in seconds, in cool/temperate conditions, for the heat intervention and control groups (Mikkelson et al., 2019).
A common observation amongst other similar studies is that blood plasma volume, and at times also Hb-mass, is enhanced via heat adaptation strategies, but without an association with performance metrics. A similar accusation has been leveled at using altitude training (see Siebenmann & Dempsey, 2020) whereby physiological adaptations do not necessarily translate to performance outcomes. Interestingly, the Karlsen et al. (2015) study found that the blood plasma volume increase was not associated with a change in peak power or time trial performance within trained cyclists. Similar outcomes have been noted by Lundby & Robach in their 2025 review, who through a series of heat training studies were able to observe an increase in Hb-mass, but not any alteration in exercise performance.
Practical Considerations
Length of Protocol
Short term heat acclimatisation of two weeks has been shown by Karlsen et al. (2015), amongst others to increase blood plasma volume. However, prolonged heat acclimatisation protocols of several weeks are required before this translates to an increase in Hb-mass (Nybo et al., 2022). Lundby & Robach’s 2025 review includes a series of heat training studies that were able to observe an increase in Hb-mass, all involving interventions of 5 weeks, with 5x or 6x sessions per week of 50-60 minutes each. Indeed, Nybo et al. (2022) recommend that, while the non-hematological adaptations may be achieved with short-term protocols (within days), the full potential and Hb-mass elevation require prolonged acclimation. They too have used ~5 weeks, with at least 5 sessions per week, to secure enough time.
This is a big commitment for many amateur athletes who are already limited on time for their training. Dedicating so long to sweating away overdressed on the indoor trainer or slumped in a sauna runs the risk of negatively impacting their other training sessions. Most of the studies have been carried out on high-level cyclists who were able to retain regular training patterns alongside the heat-adaptation protocols. If one were to just dedicate their time to heat training for five weeks, basic aerobic fitness is only going to suffer, likely beyond any gains that may be acquired through the heat.
Decay
Let’s say that you do indeed see big performance improvements through having subjected yourself to a heat adaptation protocol. You don’t want to lose those gains. However, the physiological adaptations associated with heat acclimatisation are transient in nature and steadily decay without consistent heat exposure (Périard et al., 2015).
Dunn et al. (2024) state that current evidence suggests 1 day of physiological heat adaptation is lost for every 2 days without heat exposure, and any performance adaptations will be diminished after 2 weeks without exposure. Similarly, a 2018 meta-analysis of 21 studies by Daanen et al. (2018) concluded that the rate of decay for the main adaptations following heat acclimation (lowered heart rate and core temperature) is 2.5% per day without heat exposure. Therefore, within two weeks a well-adapted individual may lose 30–35% of the heart rate and core temperature adaptations if regular heat exposure is removed.
However, these previous adaptations are non-hematological, so let us consider those with more relevance to performance in cool conditions. The aforementioned Ronnestad et al. (2022) study demonstrating improved performance also included a heat maintenance period to assess hematological parameters. Immediately after the initial 5 weeks of heat training, a 3 week heat maintenance period was commenced, which included three heat training sessions per week. They found that Hb-mass continued to increase, by 3.3% for those subjected to the maintenance period and by 0.8% for those who stopped heat training.
Similar to the previous point, 3 heat training sessions per week is still a big commitment just for maintenance. However, there is less research on the rate of decay of hematological adaptations than those more relevant for exercising in the heat solely (non-hematological). It is relevant to note that over the 3 week period in the Ronnestad et al. (2022) study, the group that stopped training did not see a decay in Hb-mass. In fact it still rose slightly. It could be hypothesised that, as these adaptations take longer to arise, they also take longer to decay. Furthermore, as Périard et al. (2021) highlight, there is support for the notion that aerobic fitness and regular exercise in cool conditions contribute to maintain adaptations or reduce the rate of decay. So maybe specific heat maintenance isn’t even required for haematological adaptations.
The ‘Training Camp Effect’
This is again an argument made to question the benefits of altitude training. As Alex Hutchinson, in one of his Sweat Science articles puts it:
“you send athletes away to an idyllic mountain resort, away from the stresses of daily life, and tell them that this is their opportunity to make a big gain in fitness. As a result, they train like animals, sleep like hibernating bears, and emerge ready to conquer the world.”
Are we seeing something similar with heat adaptation training? Nybo & Lundby (2016) raise this question, stating that the premise for concluding that heat acclimatisation improves aerobic performance in athletes exercising in cool conditions requires that there is a truly additional effect, and that the observations are not just a normal training effect or influence by the participation in a scientific study. Furthermore, the absence of a control group in several studies where athletes complete a training camp precludes the ability to adequately distinguish between the effects of heat acclimation and those of normal training on performance enhancement in cool conditions (Périard et al., 2021).
Even still, the addition of a control group to heat acclimation research studies is not straightforward, as exercise performed at a given work rate in cool conditions will elicit a lesser thermal and cardiovascular response than in the heat, making it difficult to balance the training stimulus and determine the underlying cause of any adaptations observed (i.e. whether it was the heat or just differing training loads).
Also to consider is that the transfer of benefits stemming from training in the heat to performance in cool environments (through cross adaptation) is difficult to accurately determine given the heterogeneity between the studies that have been carried out. Additionally, Nybo & Lundby (2016) highlight that, for obvious reasons, blinding is not possible in heat acclimatisation studies. Ruling out a placebo effect is thus difficult to prove.
Perhaps, with all this focus on novel modes of training and searching for the extra percentage, we are losing sight of the fundamentals. Périard et al. (2021) justifiably point out that training per se, even in cool conditions, leads to adaptations commensurate with heat acclimation. Even when undertaken in cool conditions, endurance training reduces physiological strain and increases exercise capacity in the heat, with aerobically trained individuals exhibiting lowered resting heart rate and core temperature. Any aerobic exercise can also increase total Hb-mass, enhancing oxygen-carrying capacity (see Hu & Lin, 2012).
This may even apply for the non-hematologic adaptations. A meta-analysis by Alhadad et al. (2019) examined the impact of heat mitigation strategies on lowering core temperature at the start of exercise, attenuating the rate of rise in core temperature during exercise and improving endurance performance. They found that the most influential strategy was being aerobically fit, followed by heat adaptation, pre-cooling and fluid ingestion.
Forest plot of Hedge's g weighted averages of heat mitigation strategies on endurance (Alhadad et al. 2019).
Hot Takeaways
If you are preparing to exercise in hot conditions then being adapted to the heat is only going to help, and can be gone about in a relatively short period of time. The non-hematological adaptations that help to up-regulate thermoregulatory capacity, and thus exercise capacity, happen relatively quickly and if done close to the event do not have to detract significantly from the training process.
When we are considering the hematological adaptations from heat training, the picture is less straightforward. It seems fairly well established that Hb-mass can be increased through effective heat acclimatisation protocols, likely through a pathway associated with increased blood plasma volume. However, whether this then translates to performance improvements isn’t so evident as there are studies with contradictory findings. Even in those that do find a positive association, we are generally talking about small percentage changes in short term power tests. As I always like to have at least some ultra-distance specificity, I feel obliged to repeat that short term power does not necessarily equate to success over very long aerobic efforts (FTP for show, Aerobic Threshold for an ultra pro).
Then we come to the bigger picture. Although the Alhadad et al. (2019) review was referring to heat-specific strategies, their finding that aerobic fitness was the most important factor is one which could be applied in numerous other areas. No matter the circumstances, when performing an exercise aerobically, aerobic fitness will always be the number one priority. If you have scope to improve your aerobic fitness, the potential gains will often be an order of magnitude greater than anything else. To that extent, and with the evidence available, I would place all-year heat training in the ‘marginal gains’ category.
That the protocols with evidence for hematological adaptations from heat training are so onerous (around 5x sessions per week for 5 weeks), and likely require an element of maintenance to retain the gains, makes me even more inclined to believe that this strategy could prove to be a net negative for the majority of amateur athletes. There may be no acute downside per se to doing the heat training sessions if done properly, but to see any real benefit for exercise in cool conditions, all evidence points to the need for a concerted and time-consuming effort. When this gets in the way of regular training it becomes a case of incorrect prioritisation. This could present itself through swapping sessions for heat training or adding stress to the overall load, thereby detracting from the quality of other sessions.
Maybe you are 99% of the way there and have a spare 5 hours each week burning a hole in your training schedule, plus the time to factor in additional recovery and then maintenance year-round. If so, then adopting heat training throughout the year may be for you. For the rest of us, maybe we should cool our jets.
This mindset is also seen with the likes of supplements and other ‘short cuts’ to fitness. It may not be spicy, it may not be trendy and it may not be glamorous (although neither is sweating away slumped in a sauna), but consistent training following well established principles should always come first. Dizzee may be having a hot winter, but you and I may be better off staying cool and chillin’ wiv da man dem.
References
* Rascal, Dizzee. Brand New Day. Boy in da Corner. XL Recordings. July 2023. https://youtu.be/6X_idmIH934?si=6an_iz7mBzy1b7OJ&t=10
Alhadad SB, Tan PMS, Lee JKW. Efficacy of Heat Mitigation Strategies on Core Temperature and Endurance Exercise: A Meta-Analysis. Front Physiol. 2019 Feb 13;10:71. doi: 10.3389/fphys.2019.00071. PMID: 30842739; PMCID: PMC6391927.
Daanen HAM, Racinais S, Périard JD. Heat Acclimation Decay and Re-Induction: A Systematic Review and Meta-Analysis. Sports Med. 2018 Feb;48(2):409-430. doi: 10.1007/s40279-017-0808-x. PMID: 29129022; PMCID: PMC5775394.
Dunn RA, Fry LA, Sekiguchi Y, Benjamin CL, Manning CN, Huggins RA, Stearns RL, Casa DJ. Effect of Heat Acclimatization, Heat Acclimation, and Intermittent Heat Training on Maximal Oxygen Uptake. Sports Health. 2025 Mar;17(2):305-311. doi: 10.1177/19417381241249470. Epub 2024 May 6. PMID: 38708678; PMCID: PMC11569670.
Hu M, Lin W. Effects of exercise training on red blood cell production: implications for anemia. Acta Haematol. 2012;127(3):156-64. doi: 10.1159/000335620. Epub 2012 Jan 31. PMID: 22301865.
Karlsen, A., Nybo, L., Nørgaard, S.J., Jensen, M.V., Bonne, T. and Racinais, S. (2015), Heat acclimatization time course in cyclists. Scand J Med Sci Sports, 25: 240-249. https://doi.org/10.1111/sms.12449
Karlsen, A., Racinais, S., Jensen, M.V., Nørgaard, S.J., Bonne, T. and Nybo, L. (2015), Heat acclimatization transfer to cool. Scand J Med Sci Sports, 25: 269-276. https://doi.org/10.1111/sms.12409
Lorenzo S, Halliwill JR, Sawka MN, Minson CT. Heat acclimation improves exercise performance. J Appl Physiol (1985). 2010 Oct;109(4):1140-7. doi: 10.1152/japplphysiol.00495.2010. Epub 2010 Aug 19. PMID: 20724560; PMCID: PMC2963322.
Lundby C, Hamarsland H, Hansen J, Bjørndal H, Berge SN, Hammarstöm D, Rønnestad BR. Hematological, skeletal muscle fiber, and exercise performance adaptations to heat training in elite female and male cyclists. J Appl Physiol (1985). 2023 Jul 1;135(1):217-226. doi: 10.1152/japplphysiol.00115.2023. Epub 2023 Jun 1. PMID: 37262101.
Lundby, C. and Robach, P. (2025), Altitude or heat training to increase haemoglobin mass and endurance exercise performance in elite sport. J Physiol. https://doi.org/10.1113/JP287700
Mikkelsen CJ, Junge N, Piil JF, Morris NB, Oberholzer L, Siebenmann C, Lundby C, Nybo L. Prolonged Heat Acclimation and Aerobic Performance in Endurance Trained Athletes. Front Physiol. 2019 Nov 1;10:1372. doi: 10.3389/fphys.2019.01372. PMID: 31749712; PMCID: PMC6843002.
Nybo, L. and Lundby, C. (2016), CrossTalk opposing view: Heat acclimatization does not improve exercise performance in a cool condition. J Physiol, 594: 245-247. https://doi.org/10.1113/JP270880
Nybo L, Rønnestad B, Lundby C. High or hot—Perspectives on altitude camps and heat-acclimation training as preparation for prolonged stage races. Scand J Med Sci Sports. 2024; 34:e14268. doi: 10.1111/sms.14268
Périard, J.D., Racinais, S. and Sawka, M.N. (2015), Adaptations and mechanisms of heat acclimation. Scand J Med Sci Sports, 25: 20-38. https://doi.org/10.1111/sms.12408
Périard JD, Eijsvogels TMH, Daanen HAM. Exercise under heat stress: thermoregulation, hydration, performance implications, and mitigation strategies. Physiol Rev. 2021 Oct 1;101(4):1873-1979. doi: 10.1152/physrev.00038.2020. Epub 2021 Apr 8. PMID: 33829868.
Rønnestad BR, Lid OM, Hansen J, Hamarsland H, Mølmen KS, Nygaard H, Ellefsen S, Hammarström D, Lundby C. Heat suit training increases hemoglobin mass in elite cross-country skiers. Scand J Med Sci Sports. 2022 Jul;32(7):1089-1098. doi: 10.1111/sms.14156. Epub 2022 Mar 26. PMID: 35305278; PMCID: PMC9544462.
Rønnestad, Bent R.; Urianstad, Tomas; Hamarsland, Håvard; Hansen, Joar; Nygaard, Håvard; Ellefsen, Stian; Hammarström, Daniel; Lundby, Carsten. Heat Training Efficiently Increases and Maintains Hemoglobin Mass and Temperate Endurance Performance in Elite Cyclists. Medicine & Science in Sports & Exercise 54(9):p 1515-1526, September 2022. | DOI: 10.1249/MSS.0000000000002928
Siebenmann C, Dempsey JA. Hypoxic Training Is Not Beneficial in Elite Athletes. Med Sci Sports Exerc. 2020 Feb;52(2):519-522. doi: 10.1249/MSS.0000000000002141. PMID: 31939915.